Endodontics
Endodontics
Since 1974 | Locally Owned
Quick Links:
Endodontics
Top
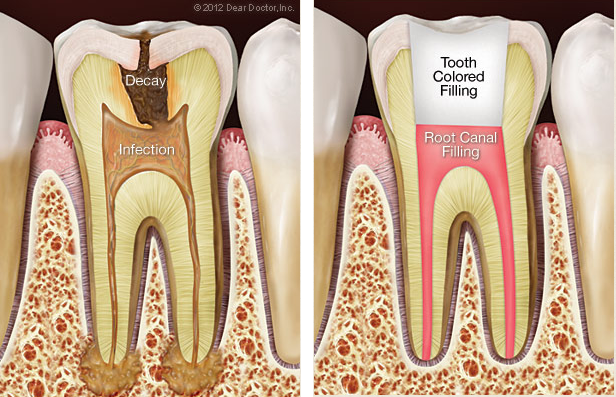
Endodontics is the dental specialty that deals with tissues and structures located inside the tooth. One of the most common endodontic treatments is root canal therapy, a procedure which effectively eases the pain associated with a bacterial infection deep within the pulp of the tooth. Of course, root canal treatment doesn't just relieve pain — it also stops the infection by removing dead and dying tissue from the tooth's pulp. Plus, it helps to save the tooth, which is in danger of being lost if left untreated.
Yet root canal therapy isn't the only treatment endodontics offers. This field also deals with cases of dental trauma, performs microsurgery on the tips of the tooth's roots, and even helps figure out what's going on when tooth pain seems to come and go intermittently, or when the pain isn't localized at one tooth. So when it comes to preserving your natural teeth, endodontics has plenty of ways to help.
The Inside Story
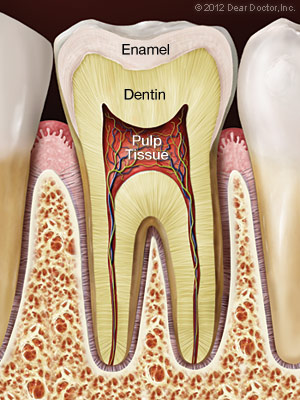
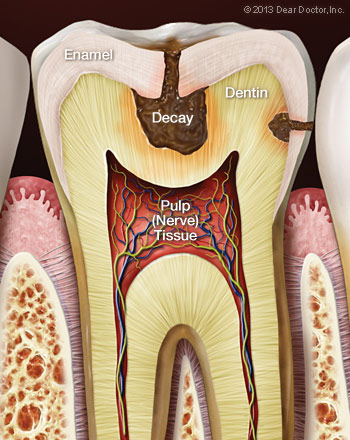
What's inside your teeth? Behind the tough, shiny enamel of the tooth's visible crown lies the sturdy inner tissue called dentin. Dentin is also found behind the cementum that forms the outer layer of the tooth's roots — in fact, it makes up the bulk of the tooth's structure. Similar in many ways to bone tissue, dentin is composed of many tiny tubules which can transmit sensations to nerve cells when it is stimulated.
At the core of the tooth, inside small, branching chambers called the root canals, we find the soft pulp tissue. This consists of nerves, connective tissues and blood vessels which extend into the center of the tooth and exit through canals near the apex (tip) of the tooth's roots. When problems (such as infection and inflammation) develop in the pulp tissue, your first indication of trouble may be tooth sensitivity — or intense pain. In time, as the nerves die, the pain may go away… but the problem won't. In fact, if left untreated, the end result may be tooth loss.
The “Root” of the Problem
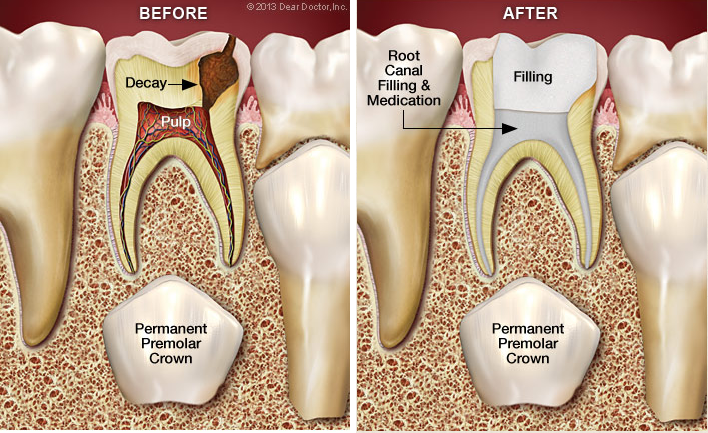
What could cause the pulp tissue to become diseased and lead to root canal problems? One potential source of infection is untreated tooth decay, which can allow bacteria from the tooth's surface to work its way deep inside. A crack or fracture in a tooth could offer another pathway for microorganisms to infect the pulp.
Dental trauma — from a sports injury, for example — may also damage dentin or pulp, or expose it to infection. Extensive dental procedures (such as multiple fillings or restorations on the same tooth) may cause trouble; occasionally, even routine procedures like orthodontics may eventually lead to root canal problems.
Endodontic Treatment
The old gag line “I'd rather have a root canal” may still get a laugh — but root canal problems are no joke. It's important to remember that root canal treatment doesn't cause pain; it relieves pain. A typical root canal procedure is performed with local anesthetics, and doesn't cause any more discomfort than having a filling. Here's what to expect:
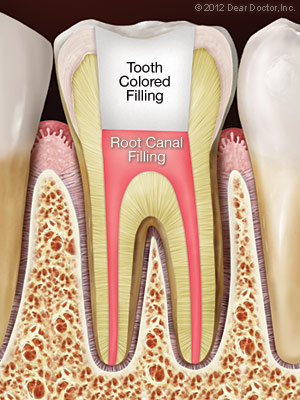
First, you will receive anesthesia (usually a numbing shot) — and for many patients, the worst is now over. Next, a small opening is made in the tooth surface to give access to the pulp chamber and root canals. Then, tiny instruments are used — often with the aid of a microscope — to remove dead and dying tissue from inside the narrow passages. These passages are then cleaned, disinfected, and filled with a safe, inert material. Finally, the opening in the tooth is sealed to prevent contamination.
Other endodontic treatments may be recommended for removing sources of infection and preventing future problems. Following an endodontic procedure, it may be necessary to have a restoration (such as a crown) placed on the tooth to restore it to full function and aesthetic appearance. After that, with proper care the restored tooth should last for many years.
Related Articles:
Combined Root Canal & Gum Problems
Top
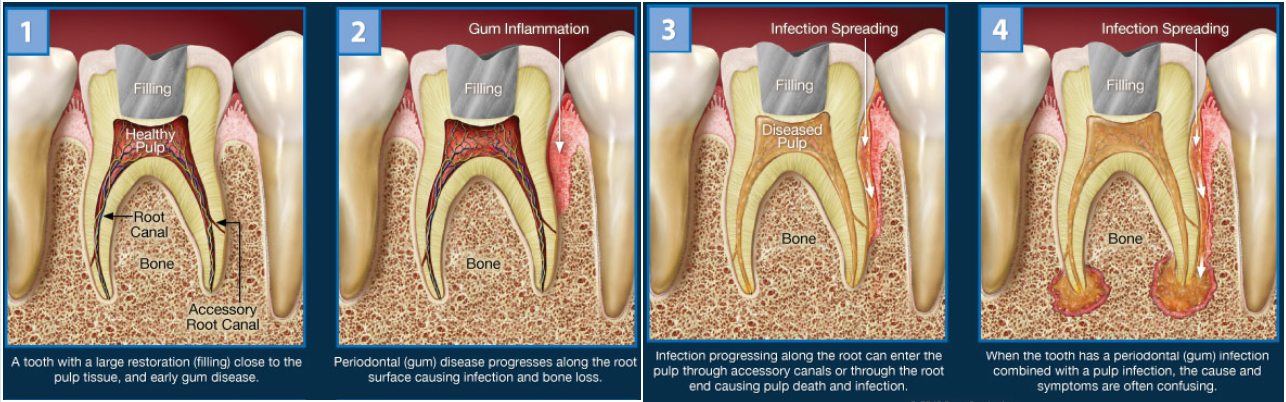
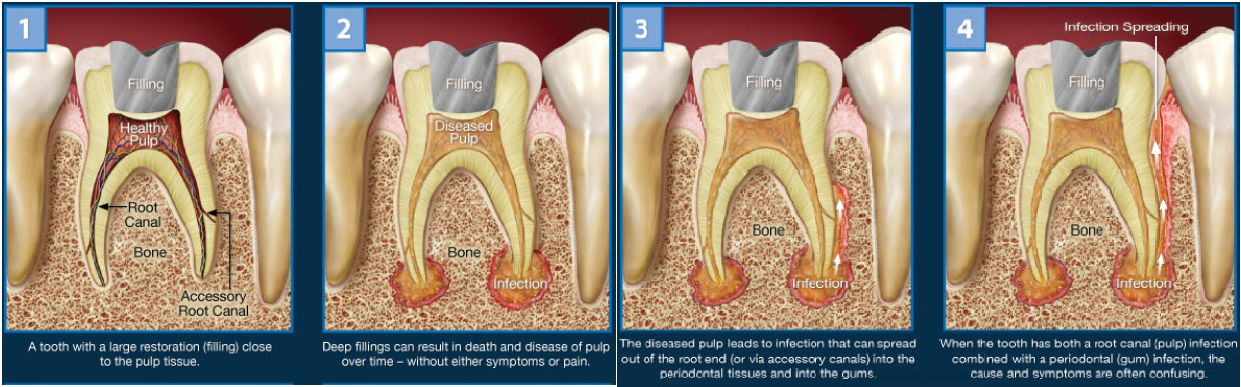
When you experience pain in your mouth, it's sometimes abundantly clear which tooth is causing it. At other times, the sensation of discomfort is more diffuse, generalized or hard to pinpoint. On occasion, it can even be challenging to determine exactly what problem or combination of problems is causing the symptoms you're experiencing. This may be the case when an infection exists in the root canals of a tooth as well as the gum tissue adjacent to it.
In this situation, the infection may have begun in the pulp of the tooth itself; or, it may have started in the gums. Over time, it has spread from one location to the other — and now it's causing a confusing set of symptoms that are difficult to sort out. Regardless of where the problem started, a thorough analysis will be necessary before treatment can begin, to give you the best chance of saving the tooth.
ROOT CANAL INFECTION LEADING TO GUM DISEASE
Confusing Symptoms
From time to time, many people experience oral discomfort that's dull or intermittent. Occasionally, a more insistent pain may be triggered by a stimulus like temperature (from hot or cold foods or beverages) or pressure (from biting down on something). Sometimes, it may feel as though the ache is coming from a group of teeth rather than one single tooth — or even from the sinus area above the back teeth.
These symptoms can indicate a number of dental issues, including root canal and gum problems, and shouldn't be disregarded. However, if you manage to ignore the acute pain, in many cases it will fade in time. But this isn't good
news: It generally means that the infected tissue in the pulp of your tooth has died, and the nerve is no longer functioning. That's when the problem may become more serious.
Chicken or Egg?
When the pulp tissue inside your tooth becomes severely infected, it's possible for the disease to move through openings at the end (apex) of the root, and outside of the tooth. It can then spread to the periodontal ligament, which anchors the tooth to the surrounding bone and gum tissue. From there, the infection may extend to the gum tissue and cause periodontal disease, or even result in a painful gum abscess. At that point, you may have pain — even severe pain that will let you know exactly which tooth is affected.
But it's also possible for the infection to be spread by the exact opposite pathway. In this case, an infection that originated in the gums (commonly due to periodontal disease caused by a buildup of plaque) may have has traveled through small passageways called accessory canals, which are located in between a tooth's roots, or on the sides of the roots. The infection can then extend into the tooth's pulp. If your teeth are fractured, it's even easier for disease to spread.
GUM DISEASE LEADING TO ROOT CANAL INFECTION
Treatment Methods
When dental problems involves both root canals and gum disease, saving the affected tooth can prove challenging. This is when it matters where the infection started: If it's primarily a root-canal problem that later moved into the gums, the outlook for the tooth is reasonably positive if it receives immediate treatment. If gum disease came first, however, the prospects often aren't as good; by the time the infection has moved into the tooth, it's possible that much bone has already been lost, making the tooth's long-term prognosis poor.
In either case, the cause of the tooth pain will need to be diagnosed and an effective treatment plan developed. The sooner that happens, the better: Root canal and gum problems simply don't get better on their own.
Related Articles:
Cracked Teeth
Top
Firmly anchored in your jaw and protected by an outer coating of tough enamel, your teeth are remarkably strong — yet it's still possible for them to chip, crack, or even break. In fact, there is some evidence that today, our teeth are developing cracks at a record rate. This may be due to the fact that people are living longer (giving teeth more time to accumulate damage), or that our stress levels are increasing (which may cause teeth clenching and grinding).
Biting on hard objects, receiving a blow to the mouth, or having large cavities (or old amalgam fillings) that weaken the tooth's structure are also common causes of tooth fractures. But no matter of the cause, there are a number of symptoms that indicate a tooth may be cracked, and several treatments we can offer, depending on the severity of the injury.
Small chips on the edges or cusps of teeth often cause no symptoms, and can be treated by cosmetic bonding or other methods. Deeply fractured teeth, on the other hand, may be a serious problem. The sooner they are treated, the more likely it is that the affected tooth can be saved. Let's take a look closer look at the types of fractures teeth can develop, and the symptoms they may produce.
Minor Cracks (craze lines)
These tiny fissures in the outer enamel of the tooth often cause few or no symptoms; in fact, most don't require treatment. If you are having tooth pain, however, these cracks will need to be evaluated and possibly treated. That's because without a careful examination, there is no way to know for sure whether these cracks go into only the enamel, or if they penetrate into the dentin (inner body) of the tooth. While the tiniest craze lines don't show up on X-rays, they can often be detected by feel (using a small instrument called an explorer), by having you close down on a “bite stick,” or by using special dye stains or high-magnification instruments.

Vertical Cracks
This type of crack often starts at the chewing surface and extends toward the roots — but may it also begin in the root and continue toward the crown. Either way, it doesn't completely separate the tooth into two parts. Depending on the extent of the fracture, you may feel only minor discomfort that occurs in response to temperature changes (with hot or cold beverages, for example); or, it may produce sharp pain when you chew. In any case, you shouldn't ignore the symptoms, because cracked teeth require dental treatment quickly to keep them from progressing further. If the cracks continue to progress, tooth extraction may become necessary.
Deep Fractures or Split Teeth
When serious fractures occur, you'll know it: The distinct parts of the tooth can be separated from each other, and tooth's pulp is often inflamed and painful. This condition requires immediate treatment, and it's rarely possible to save the affected tooth.
Treatment for Cracked Teeth
What treatment is best for a cracked tooth depends on the extent and the severity of the damage. If a small crack is detected early enough, it's often possible to seal the fissure with restorative materials. For larger cracks that involve the pulp of the tooth, root canal treatment is generally required. Afterward, the visible structure of the tooth may be restored with a crown or “cap.” Sometimes, additional procedures may be recommended to try and save the tooth. In the most severe cases, however, the tooth will need to be extracted.
The preferred treatment for cracked teeth is — you guessed it — prevention! Wearing proper protective equipment (including a custom-fitted mouthguard) when playing sports, and staying alert to dangerous situations (like distracted or impaired driving) can help keep you safe. So can regular dental checkups, where your teeth are examined carefully for early signs of a problem. However, if you experience any symptoms that could indicate a cracked tooth, don't wait: The sooner it's treated, the better the chance that we can save it.

Related Articles:
Root Canal Retreatment
Top
Most of the time, root canal therapy is effective at permanently relieving tooth pain and halting infection of the soft tissues deep inside the teeth and gums. But occasionally, as in any medical procedure, the body may not heal as we expect it to. After a period of time, you may experience pain in the affected tooth again — or, even if you have no symptoms, x-rays may reveal that infection is still present near the tooth's roots. In that case, you may need root canal retreatment.
There are several reasons why your root canal treatment may not have succeeded at first. The “canals” themselves are slender, forking passageways deep inside the tooth that enclose nerves and blood vessels: the tooth's soft “pulp.” They can be so narrow and intricate that some may have gone undetected, or failed to respond to treatment the first time. Or, the canals might have become recontaminated via a number of routes: a delayed or ineffective crown restoration, new tooth decay, advancing gum disease, or a cracked or fractured tooth. Any of these conditions could result in reinfection.
If initial root canal (endodontic) therapy has failed, the first thing to do is evaluate your options. Besides retreatment, the alternatives may include endodontic surgery or extraction (removal) of the tooth. However, a missing tooth should be replaced by a dental implant, a bridge or a partial denture as soon as possible — and none of these are simple or inexpensive options. That's part of the reason we prefer to help you retain your natural teeth whenever possible.

The Retreatment Procedure
If endodontic retreatment is appropriate for you, the procedure is similar to a routine root canal, with a few added measures. After you are anesthetized (usually with a numbing shot), any restorations presently on your tooth — crowns, for example — will be altered to provide access to the root canal filling material. This is usually accomplished by making a small opening into the inner part of the tooth, removing filling material or obstructions, and cleaning the pulp chambers with tiny instruments.
A microscope and light are used to search carefully for additional canals or unusual structures. If the treatment process becomes extremely complex, it may be finished in a subsequent visit. Finally, when all the canals have been cleaned and disinfected, they will be filled with inert material and sealed. Then a temporary filling will be placed in the tooth. A permanent restoration will need to be placed at a later time.
Is Root Canal Retreatment My Best Option?
Medicine and dentistry are as much art as science, and neither one can guarantee that any procedure will be 100% successful. While endodontic retreatment can be more complex than initial root canal therapy, it offers a good chance of success in many instances. And, since the field of endodontics is constantly evolving, it may be possible to use new techniques that weren't available when your first root canal procedure was done.
Dentists take seriously our responsibility to help you understand the risks, benefits and alternatives for treating root canal problems. When we recommend retreatment, it's because we feel it is the best way for you to preserve your natural teeth — and we want you to be able to enjoy them for many years to come.
Related Articles:
Root Canal Surgery (Apicoectomy)
Top
Occasionally, root canal treatment proves unsuccessful at resolving an infection in the tissues near a tooth's roots. That's when a minor surgical procedure called an apicoectomy may be recommended. Because this procedure is often performed with the aid of a microscope and other small specialized tools, it's considered a type of endodontic microsurgery. Probably the most common type of root canal surgery, an apicoectomy involves removing a small portion of the apex (tip) of the tooth's root, along with any surrounding hard or soft tissue that may be infected.
What would cause you to need an apicoectomy? There could be several reasons, including a canal that is blocked or inaccessible, an anatomical irregularity, or a fracture or crack in the tooth's roots. The procedure is normally only recommended after one or more root canal treatments have been attempted, and have failed. Since this type of problem generally occurs near the apex of the root, the procedure is often an effective way to treat a persistent infection.
Before an apicoectomy procedure, diagnostic images (such as X-rays) of the affected tooth and surrounding bone, a careful review of your medical history including medications you take (both prescription and non-prescription), and other factors are reviewed. If an apicoectomy is recommended, the reasons for it will be explained to you.

The Apicoectomy Procedure
Root canal surgery is usually performed under local anesthesia such as a numbing shot, so you won't feel any pain. To begin the procedure, a small incision is made in the gum, and the infection at the end of the tooth's roots is exposed. The infected tissue is then removed, along with a few millimeters of the root tip itself. A dye may be used to help make cracks or fractures easy to see; if we discover that the tooth is fractured, it may be better to extract (remove) it at this time instead of completing the apicoectomy.
Next, a microscope and light are used to examine the tiny canals. They will be cleaned with an ultrasonic instrument, then filled with an inert material and sealed up with a small filling. To finish the procedure, a small bone graft may be placed at the affected site, and then the gum tissue covering the tooth's root will be sutured (sewn) closed. X-rays may also be taken as the procedure nears completion. Afterwards, instructions on postoperative care will be given, and you'll go home. Most apicoectomies take about 30 to 90 minutes to complete.
Following the procedure, you may experience some swelling and soreness in the area that was treated. Over-the-counter non-steroidal anti-inflammatory medications (such as ibuprofen) are usually all that's needed to control any discomfort. You can probably return to normal activities the following day, but you may want to avoid eating hard or crunchy foods or brushing vigorously for a few days afterwards. If your sutures aren't self-dissolving, you will be asked to return in about a week to have them removed.
The Goal: Saving Your Tooth
Although apicoectomy is typically a safe and effective procedure, there are slight risks with any type of minor surgery. That's why apicoectomies are not recommended unless further root canal treatment won't be effective. An alternative treatment in most cases would be extraction of the tooth. However, our goal as dentists is to help you preserve your natural teeth for as long as possible.
While there are excellent methods of tooth replacement (such as dental implants), these involve further and more complex treatments, and they can be costly. An apicoectomy is generally a permanent and cost-effective solution which can help the tooth last for the rest of your life.
Related Articles:
Root Canal Treatment
Top
Root canal treatment — also called endodontics (“endo” – inside, “dont” – tooth) — is a set of specialized procedures designed to treat problems of the soft pulp (nerve) tissue inside the tooth. While some mistakenly think of it as an unusually painful treatment, in most cases the procedure is no more uncomfortable than getting a filling. It's actually one of the most effective ways of relieving some kinds of tooth pain.
A root canal procedure becomes necessary when infection or inflammation develops in the pulp tissue of the tooth. Pulp tissue consists of blood vessels, connective tissue and nerve cells — which explains why a problem here may cause you to feel intense pain. In time, the pain may go away... at least temporarily. Without treatment, however, the infection won't. It can lead to a dental abscess, and may even contribute to systemic problems in other parts of the body.
Root Canal Treatment Is Your Friend
We've all heard the gag: “I'd rather have a root canal...” This comedy line, comparing the procedure to something truly undesirable, may be funny — but putting off needed endodontic treatment is no joke. The idea that a root canal procedure invariably comes with complications and pain is a shopworn myth. It's certainly true that infection or inflammation in the tooth's pulp can be excruciatingly painful. But you should remember that having a root canal results in eliminating this acute pain and is not the cause of the pain.
Need another reason not to delay root canal treatment? How about this: A natural tooth that's saved via root canal treatment and restoration helps you avoid the problems that commonly occur when teeth must be removed. These include unwanted tooth migration or shifting, which can lead to difficulties in chewing; the need for bridgework or dental implants, which may be costly and complicated; and even the eventual loss of bone structure from the area of the missing tooth.
Causes of Root Canal Problems
Root canal problems stem from infection and inflammation of the tooth's pulp tissue. One potential cause of infection is deep tooth decay. Untreated dental cavities eventually allow bacteria to work their way down to the center of the tooth, where they may infect the pulp tissue. Another path by which bacteria may come into contact with pulp is via chipped or cracked teeth. Any opening in the protective enamel coating has the potential to allow bacteria access to the tooth's pulp.
Trauma to the tooth — the kind that might result from a sports injury or automobile accident, for example — is also a major cause of pulp tissue damage. In this case, it's essential to seek treatment immediately, both to try and save the tooth, and to prevent future problems.
In some cases, extensive dental work itself may cause damage to the pulp tissue that will need to be treated via a root canal. Having multiple fillings or restorations on the same tooth increases the chances of this type of injury. Occasionally, common procedures like crown preparation or orthodontics may eventually lead to root canal problems.
What to Expect During Root Canal Therapy
If an examination shows that you do need root canal therapy, don't worry — it's one of the most routine and effective procedures in the arsenal of dental treatments and can often be accomplished in just one visit.
The root canal process generally begins the same way as a filling does, and with no greater discomfort: an anesthetic is administered to numb the tooth and the surrounding area. For many patients, the worst is already over.

Next, a small opening is made in the surface of the affected tooth to give access to the pulp chamber and root canals. Tiny instruments are used, sometimes with the aid of a microscope, to remove the dead and dying pulp tissue from inside these narrow passageways. The chamber and empty canals are then cleaned, disinfected, and prepared to receive a filling of inert, biocompatible material. Finally, adhesive cement is used to seal the opening in the tooth, preventing future infection.
Following root canal treatment, your tooth may feel some sensitivity or tenderness for a few days. Over-the-counter pain relievers like ibuprofen are generally effective in relieving discomfort, but prescription medications may also be given if needed. During this period, it may help to avoid biting hard on the affected tooth. All of these symptoms, however, should be temporary.
To further protect the tooth and restore it to full function, it's usually necessary to have a crown or other restoration placed on it. Restorations can take many forms, from traditional gold crowns to tooth replicas made of high-tech tooth-colored material. In any case, you will have made an investment in preserving your dental health for years to come.
Signs & Symptoms of Root Canal Issues
How do you know when you need a root canal? Sometimes, it's painfully obvious. If you feel constant and severe pain and pressure in your mouth, or noticeable swelling and extreme sensitivity in your gums, then it's clear you need an evaluation and treatment right away. Another telltale symptom of pulp tissue damage is sharp pain when you bite down on food. Lingering pain after eating hot or cold foods is also an indication of potential trouble. If you notice any of these symptoms, you need to have an examination as soon as possible.
Related Articles:
Root Canal Treatment FAQs
Top
If you have been told you need root canal treatment, you may be feeling a bit nervous. Not to worry — treating root canal problems is a routine part of dentistry that can relieve certain kinds of tooth pain and help your teeth last longer. As you learn more about this beneficial procedure, you will understand why it's needed — and how it will leave you in far better shape than you were. Here are some answers to frequently asked questions.
What is a root canal?
Dentists use the term “root canal” in referring to the tiny, narrow passageways that branch from a central, hollow space in your tooth (called the pulp chamber) down to the ends of the tooth roots. The term can also be used as a shorthand for “root canal treatment” — that is, the procedure used to save the tooth if the soft tissue deep inside of it (called pulp) becomes acutely inflamed or infected.
Why do I need root canal treatment?
If tooth pulp becomes acutely inflamed or infected because of decay or injury, the tissue will need to be removed in order to save the tooth and stop the infection from spreading. As an adult, you don't actually need the pulp — its primary use is to aid in tooth development during childhood.
Is there an alternative?
You could have the whole tooth extracted, but it's always better to try to save it — especially since root canal treatment is routine and has a very high success rate (over 90%). Saving the tooth can prevent other troubles from occurring later on; these could include bite problems from teeth shifting position, difficulty eating, and loss of jawbone volume and density.
Is root canal treatment painful?
The procedure normally causes no more discomfort that a filling would. Root canal treatment may have a bad reputation, but it is undeserved; in this case it's the disease that's to blame and not the cure. In other words, the infections that make the treatment necessary in the first place are often painful because they are inflaming tissue that has lots of nerves and therefore is very sensitive. Root canal treatment actually relieves this pain!
What will happen during the procedure?
After numbing the area, a tiny hole in the crown (top) of your tooth is made to access the pulp chamber and canals. The diseased tissue is removed, and the pulp chamber and the canal(s) are disinfected all the way to the root end(s). Teeth in the front of the mouth have one root and generally one canal; back teeth have two or three roots and generally three or four canals. Those canals andthe pulp chamber are filled with an inert, biocompatible material, and sealed with adhesive cement. The access hole will receive a temporary filling.
What will happen afterwards?
Your tooth may feel sensitive for a few days, but any discomfort can usually be relieved with over-the-counter pain medication or anti-inflammatories like ibuprofen. You will be instructed to avoid chewing on that tooth until it receives its permanent filling, which can be placed a few days later. Depending on how damaged the tooth was to begin with, it may need a full-coverage crown. Those options will be discussed with you.
How can I avoid the need for root canal treatment in the future?
Keep your teeth decay-free by brushing and flossing every day. Eat a healthy diet low in sugar and avoid acidic beverages such as soda. Have regular professional cleanings and exams. And if you're active in sports, consider ordering a custom-made mouthguard to protect your teeth from injury.
Related Articles:
Root Canal Treatment for Children
Top
Root canal treatment is a safe and effective way to stop many kinds of tooth pain, and to keep a tooth from being lost due to decay or injury. But if a root canal is recommended for your young child, you may wonder why: Isn't that baby tooth going to fall out in a few years anyway?
That's true — the primary (baby) teeth typically are shed between the ages of 6 and 12 years. Yet there are some good reasons for trying to save baby teeth for as long as possible with root canal treatment, rather than simply extracting any that are damaged by trauma or infection.
For one, primary teeth have the same functions as adult teeth — and a missing tooth at any age can cause problems with speech and eating. Baby teeth also have another important role: They serve as guides for the proper placement of the permanent teeth. Without primary teeth to guide them in, permanent teeth tend to emerge in a crooked fashion, often becoming tilted or crowded because of inadequate space. This can result in bite problems that may require extensive orthodontic treatment later.
Saving The Tooth Is Always Best
Unlike its hard outer surface, the soft pulp inside the tooth is rich in blood vessels and nerves. Problems in this area are often signaled by tooth sensitivity and pain. When these symptoms occur, radiographs (x-rays) are often necessary to confirm that the pulp is diseased, or dying. That's when treatment is needed, before an abscess or further infection can develop.
In severe cases, the tooth may need to be removed, and a space maintainer installed to fill the gap. But many times, space maintainers don't fully restore the tooth's functionality. Plus, they are susceptible to coming loose and must be monitored constantly. If possible, other treatment methods are preferred, such as:
Indirect pulp treatment. If pulp damage is minimal, it's possible to remove most of the decay (but not the pulp), apply an antibiotic, and then seal the tooth up again; that's referred to as an “indirect” treatment.
Pulpotomy. Alternatively, if decay is limited to the upper portion of the pulp, we may recommend a “pulpotomy.” This involves removing the damaged part of the pulp, stabilizing the remaining healthy portion, and then disinfecting and sealing the tooth. This “partial” root canal is a time-tested technique that's successful in many cases.
Pulpectomy. If pulp tissue is infected through the entire tooth structure, a pulpectomy may be needed, which requires the removal of all pulp tissue. The canals are then disinfected, shaped, then filled and sealed with inert material. Afterwards, the crown (visible part) of the tooth will be restored. This resembles traditional root canal therapy, with a crucial difference: The sealant we use in children is capable of being dissolved by the body. That way, when it's time for a permanent tooth to erupt, the baby tooth's roots can be naturally absorbed and tooth development can proceed normally.
Preparing for Your Child's Root Canal Treatment
As you probably already know, most of the legends you may have heard about root canal therapy simply aren't true. In fact, the procedure generally causes little discomfort, but is quite successful in relieving tooth pain! Dentists are adept at using anesthesia to block the sensation of pain, and are experienced in calming the fears of young ones. While it's understandable that you may be nervous, it will help if you don't let your child pick up on your own anxiety. A calming voice and a gentle touch can do much to relieve stress.
After a thorough examination, the best options for your child's treatment will be recommended. These procedures are routine and follow-up instructions will be provided. A root canal is nothing to fear: Think of it as a treatment that may save your child from some tooth pain now, and potentially a lot of corrective dental work later on.
Related Articles:
Tooth Sensitivity
Top
If your teeth seem especially sensitive after you brush them or when you consume certain foods or beverages, you're hardly alone: By one estimate, around 35 percent of the U.S. population experiences some degree of tooth sensitivity. While the difference between sensitivity and pain may be somewhat blurry, we can say that sensitive teeth usually produce discomfort in response to a stimulus like temperature, pressure, or even the sweetness of particular foods. What causes tooth sensitivity — and what should you do about it?
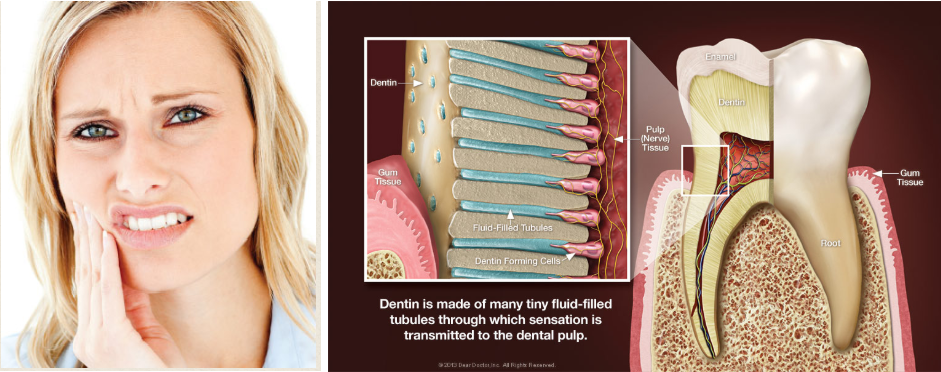
Tooth Anatomy 101
Dentin is a sturdy, calcified tissue, that can't usually be seen. It's normally covered by super-hard enamel on the visible part of the tooth (the crown), and by softer tissue called cementum on the tooth's roots (which typically lie below the gum line). The dentin itself is composed of many tiny tubules. When these tubules become exposed to the environment of the mouth, tooth sensitivity and pain may result.
There are several reasons why the dentin can become exposed. For one, the gums may recede (shrink down), revealing some of the tooth's root surfaces. This can be caused by genetic factors, periodontal disease, excessively vigorous brushing — or a combination of all three. This problem may be worsened if the tooth's roots weren't completely covered by cementum during their development, as sometimes occurs.
Another factor that may contribute to sensitivity is the erosion of tooth surfaces due to excessive acid in the diet. While acids occur naturally in the mouth, habitually drinking sodas and sports drinks can severely erode teeth — and brushing soon after you drink actually worsens the effect. That's because these acids soften the outer surfaces of the teeth, and brushing then makes it easy to wear them away. It's best to wait for an hour afterwards, to give your saliva a chance to neutralize the acid.
Tooth decay can also cause sensitivity. Decay may not only expose dentin, but can work its way down to the nerves themselves — at which point, your pain level may escalate. And sometimes, even dental work itself can cause sensitivity. Because the same tooth structures are involved, it may sometimes take a few days after a cavity is filled, for example, for a tooth to “calm down.”
Dealing With Tooth Sensitivity
What can you do about sensitive teeth? If it's a relatively minor irritation, try not to brush the affected teeth too long or hard. Make sure you're using a soft-bristled brush and the proper, gentle brushing technique. Always use a toothpaste containing fluoride, as this ingredient is proven to increase the strength of tooth enamel, which helps resist erosion. You can also try a toothpaste with ingredients designed especially for sensitive teeth, such as potassium. Studies show that these can be effective… but it may take approximately 4 – 6 weeks for you to notice the difference.
If sensitivity persists, however — or if your tooth pain becomes more intense — don't wait to get an examination to determine what's causing the problem. Once diagnosed, the most appropriate way to reduce the sensitivity will be recommended. Some treatments may include concentrated fluoride varnishes, prescription mouth rinses, or materials that are bonded to the outer surfaces of teeth. But tooth sensitivity may also be an early warning sign of other dental problems — and the sooner they're taken care of, the better off you'll be!
Related Articles:
Whitening Traumatized Teeth
Top
Teeth whitening is one of the most popular cosmetic dental treatments — and it's easy to see why. Having whiter teeth can make you look years younger, and the procedure itself is among the most conservative (and cost-effective) cosmetic treatments dentistry offers. Sometimes, however, achieving a pleasing, even shade of lightness can be challenging; this is particularly true when a tooth that needs to be lightened has been subjected to an injury (dental trauma) in the past.
Dental trauma encompasses any damage to the tooth that's caused by an external agent, whether accidental or intended. It may be due to a fall, a sports injury — or even a past orthodontic procedure. According to some studies, around a quarter of Americans aged 6 to 50 years old have experienced some traumatic dental injury, with most occurring before age 19. Traumatized teeth may react to whitening procedures differently from undamaged teeth, which can make them difficult to treat.However, several effective treatments are available.
Diagnosing a Discolored Tooth
The first step in the process of lightening a traumatized tooth is a thorough exam to find out what's causing the dark staining — and one of the first things we will determine is whether or not the tooth's pulp is “vital,” or alive. This is readily revealed by radiographs (x-rays) or other tests. If the tooth is still vital, external bleaching can often yield satisfactory results — even if it's just one tooth that needs to be whitened. In-office treatments or take-home trays are effective, but office procedures generally take much less time to produce good results.
In many cases, however, discoloration of a traumatized tooth is itself an indication that the nerves in the tooth's pulp have died. In this case, before whitening treatment can start, a root canal procedure will be necessary to remove the dead or dying tissue and prevent infection. It can also happen that a tooth that appeared normal will begin to discolor many months (or years) after a root canal has been performed. In either situation, it may be possible to whiten a non-vital tooth with a procedure called internal bleaching.

Whitening From the Inside Out
Because a non-vital tooth's stains are intrinsic (inside, rather than outside, the tooth), we need to put the bleaching agent itself inside the tooth. Internal bleaching is a routine procedure, here's how it works:
Access to the pulp chamber (the small passageway in the tooth's center) will be gained by making a small hole in the back of the tooth. Then, any debris from the chamber will be removed and rinsed away, and a special cement will be added to prevent the bleaching agent from leaking into the tooth's roots.
Next, some bleaching agent (commonly sodium perborate) will be placed in the empty pulp chamber, and temporarily seal it in. At this point, you can get up and leave the office… which is why this procedure is sometimes called the “walking bleach” technique. However, you'll return in a few days for another round of bleaching; it may take up to four visits to get the degree of lightening you want.
When the tooth reaches the desired color change, a more permanent restoration will be placed on the tooth to seal that little hole — usually a tooth-colored filling material of composite resin. Many times, this relatively conservative procedure will give your tooth all the lightening it needs. If it's not enough, the tooth can be bleached externally as well, or you can even consider a veneer or crown. The goal is to recommend the most appropriate cosmetic dental procedure, and get you the best possible results.
Related Articles:
Our Facebook Feed
Privacy Policy
| Do Not Share My Information
| Conditions of Use
| Notice and Take Down Policy
| Website Accessibility Policy
© 2025
The content on this website is owned by us and our licensors. Do not copy any content (including images) without our consent.


